Breaking the Stigma: Lung Cancer Beyond Smoking
Breaking the Stigma: Lung Cancer Beyond Smoking
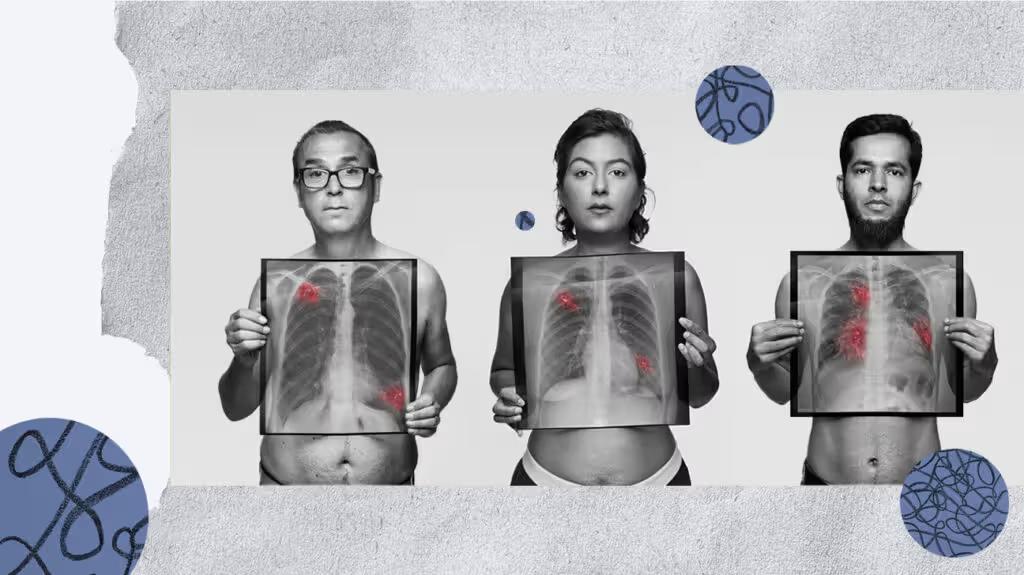
Lung cancer is a grave concern worldwide, accounting for approximately 20% of cancer-related deaths. While it is well-known that smoking is a significant cause of lung cancer, it is often overlooked that 15-20% of cases occur in nonsmokers. This subset of lung cancer is attributed to a nonhereditary gene mutation that develops later in life, resulting in a specific type of lung cancer known as EGFR positive (EGFR+) lung cancer. In this article, we will explore the latest developments in lung cancer research and treatment, shedding light on the fact that lung cancer is not just a disease of smokers.
The Impact of Smoking on Lung Cancer
According to Cancer Research UK, smoking is responsible for 72% of lung cancer cases and a staggering 86% of lung cancer deaths in the United Kingdom. Similarly, the Centers for Disease Control and Prevention (CDC) in the United States report that up to 90% of lung cancer deaths are associated with smoking. It is crucial to emphasize that quitting smoking or not starting in the first place significantly reduces the risk of developing lung cancer.
However, it is essential to recognize that not all lung cancer cases are linked to smoking. As the number of smoking-related lung cancers begins to decline, there has been a notable increase in nonsmoking-related lung cancer cases. Lung cancer is a disease characterized by the uncontrolled growth and spread of abnormal cells in the trachea, bronchi, or lung tissue. The two main types of lung cancer are small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC). NSCLC accounts for approximately 80-85% of all lung cancers and can be further divided into three main types: adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
The Rise of EGFR+ Lung Cancer

EGFR+ lung cancer is a specific form of lung cancer, primarily adenocarcinoma, that is not caused by smoking but rather by a mutation in the epidermal growth factor receptor (EGFR) gene. The EGFR mutation leads to constant cell division, resulting in the development of malignancies or cancer. The American Lung Association (ALA) estimates that EGFR+ mutations occur in around 10-15% of lung cancer cases in the United States. The most common EGFR mutations are EGFR 19 deletion, EGFR L858R point mutation, and the less common Exon 20 insertion mutation.
Interestingly, EGFR+ lung cancer is more prevalent in women than men and is more likely to be diagnosed in younger individuals and those who have never smoked or have been light smokers at some point in their lives. This suggests that EGFR+ lung cancer may contribute to the increasing incidence of lung cancer in younger women.
Recognizing the Symptoms of Lung Cancer
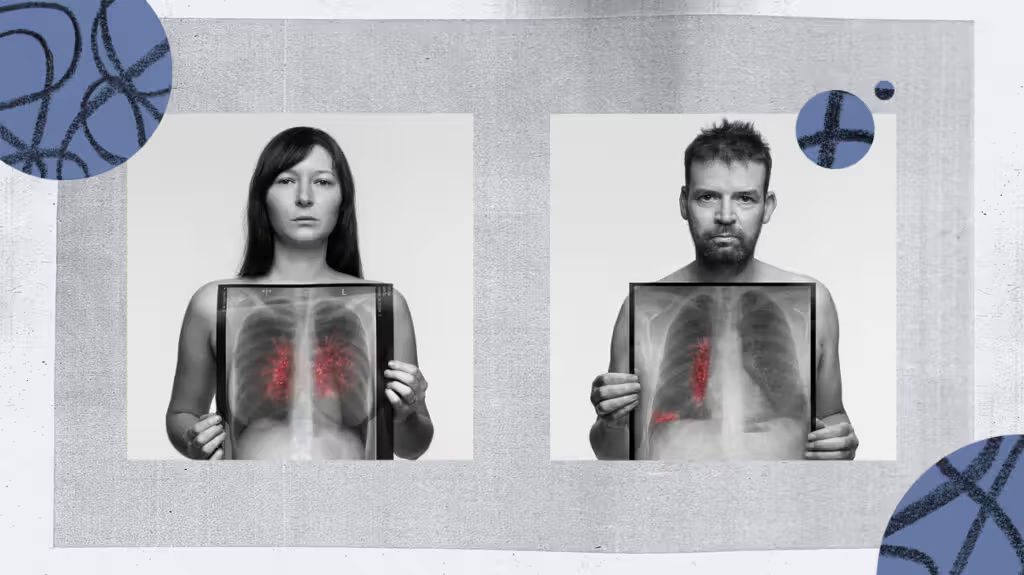
While it is commonly believed that lung cancer primarily presents with coughing and breathing difficulties, the symptoms can vary, especially in the case of EGFR+ lung cancer. Prof. Robert Rintoul, a professor of thoracic oncology at the University of Cambridge, emphasizes that individuals with EGFR+ lung cancer who are nonsmokers or light smokers may not initially consider lung cancer when experiencing symptoms. This delayed recognition often leads to the presentation of more advanced stages of the disease. It is crucial for everyone, regardless of smoking history, to be aware of potential symptoms such as persistent cough, recurrent chest infections, coughing blood, unexplained weight loss, fatigue, chest pain, and unexplained breathlessness.
Dr. Gini Harrison, a psychologist and EGFR+ lung cancer survivor, shares her own experience, highlighting that not all individuals with EGFR+ lung cancer exhibit the typical symptoms. In her case, she only experienced severe shoulder pain, with no breathing issues or wheezing. This underscores the need for healthcare providers to consider musculoskeletal symptoms, including back, chest, or shoulder pain, as potential indicators of lung cancer, particularly EGFR+ lung cancer.
Addressing the Stigma
Lung cancer research has historically suffered from a lack of funding, despite being the most common cancer in men and the second most common cancer in women. Lung cancer receives disproportionately low investment compared to its overall burden, with only 5.3% of total cancer research investment dedicated to lung cancer between 2016 and 2020. The stigma associated with lung cancer, primarily due to its strong association with smoking, may contribute to this funding disparity. Approximately 80-90% of lung cancer deaths are attributed to smoking, leading to the assumption that the disease is solely a consequence of poor lifestyle choices.
However, it is crucial to challenge this viewpoint and break the stigma surrounding lung cancer. Lung cancer can affect anyone with lungs, regardless of smoking status. By raising awareness and dispelling the stigma, we can foster greater visibility, fundraising, support, and research funding. Ultimately, this will lead to better detection of symptoms, improved treatment options, and enhanced survival outcomes.
Early Detection and Improving Prognosis
Early detection is key to improving the prognosis for individuals with lung cancer. The American Cancer Society reports that those diagnosed with localized non-small cell lung cancer have a 65% chance of surviving for five years. However, if the cancer has already spread to other parts of the body at the time of diagnosis, the five-year survival rate drops to just 9%. Despite these statistics, advancements in targeted therapies have significantly improved the outlook for individuals with all types of lung cancer.
Targeted therapies for non-small cell lung cancer depend on the stage of the cancer. In cases where the cancer is detected early, it may be possible to remove it entirely through surgery, photodynamic therapy, laser therapy, or brachytherapy. As the cancer progresses and spreads, more intensive treatment approaches such as surgery followed by radiation therapy, immunotherapy, and chemotherapy may be necessary. Genetic testing plays a crucial role in identifying gene mutations, such as EGFR mutations, to guide targeted therapy selection.
EGFR+ lung cancer is specifically treated with a group of drugs known as tyrosine kinase inhibitors (TKIs), which inhibit the enzymes responsible for activating proteins like EGFR. There are currently five approved TKIs for EGFR+ lung cancer treatment: Tarceva, Gilotrif, Iressa, Vizimpro, and Tagrisso. These medications have shown tremendous efficacy in improving survival rates and quality of life for individuals with NSCLC and EGFR mutations. However, it is important to note that the effectiveness of TKIs can vary between patients, and resistance to these drugs can develop over time. In such cases, alternative treatments like chemotherapy, radiation therapy, or other targeted therapies may be explored.
Advancements in EGFR+ Lung Cancer Research
Despite the funding challenges faced by lung cancer research, there have been notable breakthroughs in the field, particularly in the study of EGFR+ lung cancer. Recent research has identified the gene CD70 as a potential therapeutic target for individuals with resistant EGFR+ lung cancer. CD70, known for its role in promoting cell survival and invasiveness, has also been implicated in the development of other cancers, such as glioblastoma. Additionally, early-stage research has shown promise in the development of a vaccine to prevent the development of common EGFR mutation-driven lung tumors by activating immune cells. These advances highlight the potential for targeted, combined therapies in the future of lung cancer care.
Hope for Exon 20 EGFR+ Lung Cancer
Individuals with the rarer Exon 20 mutation EGFR+ lung cancer have recently received a glimmer of hope. The PAPILLON clinical trial data presented at the European Society for Medical Oncology (ESMO) Congress in Madrid revealed a new first-line therapy for patients with EGFR exon 20 insertion mutations. The combination therapy of amivantamab, pemetrexed/ALIMTA, and carboplatin has shown transformative potential in improving the treatment outcomes for this specific patient population. This breakthrough offers a new avenue for personalized medicine and underscores the importance of ongoing research and clinical trials in advancing lung cancer care.
Addressing Disparities in Care
While advancements in lung cancer treatments bring hope, it is essential to acknowledge the disparities in care and access to innovative therapies. Discrepancies exist not only within countries but also between different regions globally. Dr. Harrison highlights the significant disparity in access to clinical trials and innovative treatments between the United States and the United Kingdom, underscoring the need for patient advocacy and raising awareness to address these challenges. By empowering patients to be advocates for themselves and navigating the healthcare system, we can strive for equitable access to life-saving treatments and better outcomes for all individuals affected by lung cancer.
A Promising Future
The landscape of lung cancer is continuously evolving, with improved survival rates and better treatment options emerging. Targeted therapies, immunotherapies, and ongoing research efforts hold great promise in transforming lung cancer into a chronic, controlled illness with long-term survival achievable for many individuals. As we challenge the stigma surrounding lung cancer and allocate more resources to research, we can continue to push the boundaries of medical knowledge and provide hope to those affected by this devastating disease.
In conclusion, lung cancer is not just a smokers’ disease. While smoking remains a significant risk factor, a notable percentage of lung cancer cases occur in nonsmokers. EGFR+ lung cancer, driven by specific gene mutations, affects individuals regardless of smoking history. By raising awareness, challenging stigma, promoting early detection, and supporting ongoing research, we can strive for better outcomes, improved treatments, and ultimately, a brighter future for those impacted by lung cancer.